Hospital bosses have blamed an NHS strike for failings in the care of a 57-year-old who died following a series of health complications after a fall.
An inquest into the death of Yvonne Brown was told that a strike by junior doctors and consultants at the Norfolk and Norwich Hospital (N&N) "undoubtedly caused a deficit of interaction" with her family, as well as "missed opportunities".
It meant communications with her husband, Kelvin Millward, broke down and he only discovered she had undergone a major operation to have her colon removed when he was summoned to her bedside as her condition deteriorated. She died hours later.

Mr Millward told the hearing: “Communication of staff was abhorrent; it really was disgusting.”
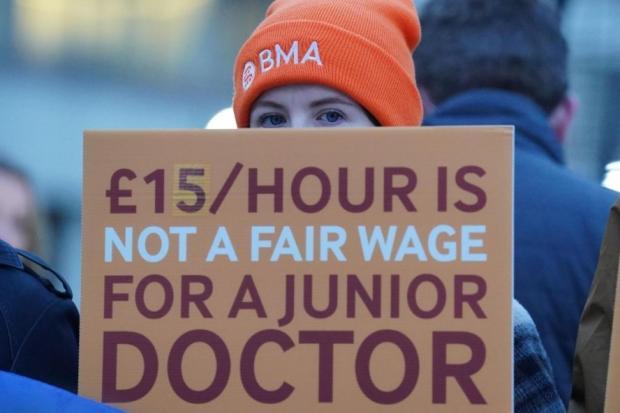
Strikes in the NHS started in December 2022, with junior doctors holding the first of 10 strikes in March 2023 in their dispute over pay.
The ongoing industrial action has led to more than 1.4 million operations and appointments being cancelled and some analysis has linked it to higher death rates.
Mrs Brown's inquest, at Norfolk Coroner’s Court, was held on the same day that the British Medical Association - which is calling for a 35pc pay rise - announced it would continue its industrial action.
The hearing was told Mrs Brown was admitted to the N&N after a fall at home in Briston, near Holt, on August 9.
Between then and her death, on September 29, there were two four-day strikes at the hospital, the first by junior doctors and the second by junior doctors and consultants.

'POOR TREATMENT'
While in hospital Mrs Brown had three more falls.
Mr Millward told the inquest: “I found this to be unbelievable considering she had just attended the hospital for that exact same reason – and that steps to prevent this from happening would have been put into place immediately on her arrival.
“This is my opinion was a clear case of negligence on behalf of the hospital staff in their failure to protect my wife while in their care.
“It’s unforgivable this was allowed to happen.”
He also witnessed while on a video call, his wife lying “uncovered on the bed with her midriff exposed.”
“This was without any nurses in sight – she must have been embarrassed and freezing.
“By now I was getting seriously concerned about my wife’s care.
“Communication of staff was abhorrent; it really was disgusting.”
'A GOOD TEAM'
Before her hospital admission, Mrs Brown had suffered with weakness in her left leg and arm for around 18 months which caused her to fall frequently.
Despite these difficulties, Mr Millward said his wife “remained upbeat and cheerful”.
He added: “As a good team, we were coping well – until that final fall at home.
“While she was in hospital, communication between my wife and I was entirely dependent on the use of mobile phones.
"It was absolutely vital both to us, but the result would lead to serious problems.”
Mr Millward explained how his wife was transferred to several wards during her stay.
He said: “It was becoming difficult to say the least to ascertain exactly what was going on at any given time – and to what treatment she was receiving – as my wife’s level of concertation and remembering details was seriously failing.
“And as a result, this led me to making numerous attempts to contact the hospital to gain information and any updates on my wife's condition.”

SURPRISE PHONE CALL
Mr Millward said he received only a handful of calls to update him on her condition during her seven-week stay, despite leaving several messages.
One of these calls was at 4am on September 29, when he was advised to make his way to the hospital after his wife’s condition began to deteriorate.
It was only after arriving at her bedside, that he was told she was recovering from having her colon removed
"This was all unbeknown to me- they did not even inform me about the procedure taking place.
“This led to my uncontrollable sobbing as to the thought of my wife being frightened, alone, and confused without me being by her side to comfort and assure her during this ordeal.”
He was also informed that she had contracted Covid-19.
“She was isolated for almost four years at home,” he added.
“Imagine spending four years trapped inside your home and being vaccinated, only to catch it from staff in a hospital - despite being isolated in a side room with no visitors.”
She died shortly after Mr Millward arrived.
He claims his wife was too unwell to consent to the operation.
In a statement to the inquest, Richard Wharton, a consultant, described her as having the capacity to understand.
He did concede that the industrial action was a factor in how she was managed and how they dealt with the family, but was not ultimately responsible for her death.
He added: “Although protocols and strategies were employed to mitigate the effect of doctor strikes, the strikes undoubtedly had an effect on our ability to manage patients.
“However, in this case, it is my opinion that her care and outcome were not affected by the strikes."
He also said that if the hospital had been "better resourced" Mrs Brown should have gone straight to an intensive therapy unit after her operation.

Assistant coroner for Norfolk, Christopher Leach, said: “Mr Wharton offered the view that doctor’s strikes had undoubtedly had an effect on their ability to manage patients."
He added: “Mr Wharton’s evidence accepted a deficit of interaction with Mr Millward. He commented that a subsequent review had identified that this may have been as a result of the junior doctors' strikes on September 19 and 22, 2023.”
Summing up the evidence to the court, based at County Hall in Norwich, Mr Leach outlined the findings of the N&N’s Structured Judgement Review - a method of reviewing the quality and safety of patient care and treatment.
He said: “The review accepted that in some respects Mrs Brown had received poor treatment at the N&N.
“It noted that there had been poor communication with Mr Millward, and noted the lack of capacity assessments.
“It indicated that it was not possible to say if the outcome would have been different but opportunities for improvement of care were identified. There were missed opportunities to discuss ceilings of care for Mrs Brown.”
Mr Leach did acknowledge that the surgery had been in her best interest.
The medical cause of death was given as hospital acquired pneumonia and Covid-19 due to, or because of, subtotal colectomy and ulcerative colitis.
He recorded a brief narrative conclusion and said: “Yvonne Brown died from pneumonia and Covid, which were acquired during hospital admission following a fall at home, and during which a pre-existing colon condition deteriorated and required surgical intervention.









Comments: Our rules
We want our comments to be a lively and valuable part of our community - a place where readers can debate and engage with the most important local issues. The ability to comment on our stories is a privilege, not a right, however, and that privilege may be withdrawn if it is abused or misused.
Please report any comments that break our rules.
Read the rules hereLast Updated:
Report this comment Cancel